Parkinson's disease (PD) is not limited to the brain, as we have known for a while. It is a widespread neuronal disorder involving not only the central nervous system. Increasing evidence also points to the gut-brain axis which connects the central and enteric nervous system (ENS). Inflammation in the ENS can trigger PD, scientists believe.
To study the enteric nervous system (ENS) a model system, which was developed recently, is most suitable. This 'ENS on a dish' uses embryonic stem cells (hESCs) which are induced to become enteric neurons and glial cells. The model system is highly suited to study the immunometabolism of the enteric glial cell. A team consisting of Paula Perez Pardo, Aletta Kraneveld and Celia Berkers applied for an ICI grant to set up this system and perform the study.
Anastasia Markidi was doing her master's in the same group. Coming from Greece where studying pharmacology usually means you will run your own pharmacy eventually, she was more interested in immunology and neuroscience. She jumped at the chance to study these fundamental aspects of PD in the ICI PhD project. "I found the proposal really interesting and they were doing exciting experiments in the lab."
ENS on a dish
Anastasia started with reproducing and testing the protocol to make the ENS on a dish. She then managed to isolate the enteric glial cells that she wanted to study because these play an important role in neuroinflammation and neuronal function. She was able to model the activation of these cells and cause inflammation by exposing them to proinflammatory cytokines.
Based on earlier results, the researchers hypothesized that particular acids such as butyrate and acetate that bacteria produce could prevent inflammation. Adding these compounds indeed stopped the induced inflammation. To know more about the fate of these acids, Anastasia labeled them with 13C and traced them with metabolomics techniques. "It was really cool to see where they end up in the cells."
Next, Anastasia wanted to model a more realistic situation. Parkinson's disease is a chronic condition characterized by a chronic, low grade inflammation. "We therefore exposed the cells to a lower dose of cytokines for longer," explains Anastasia. She expects the results of this study soon.
Alpha-synuclein aggregates
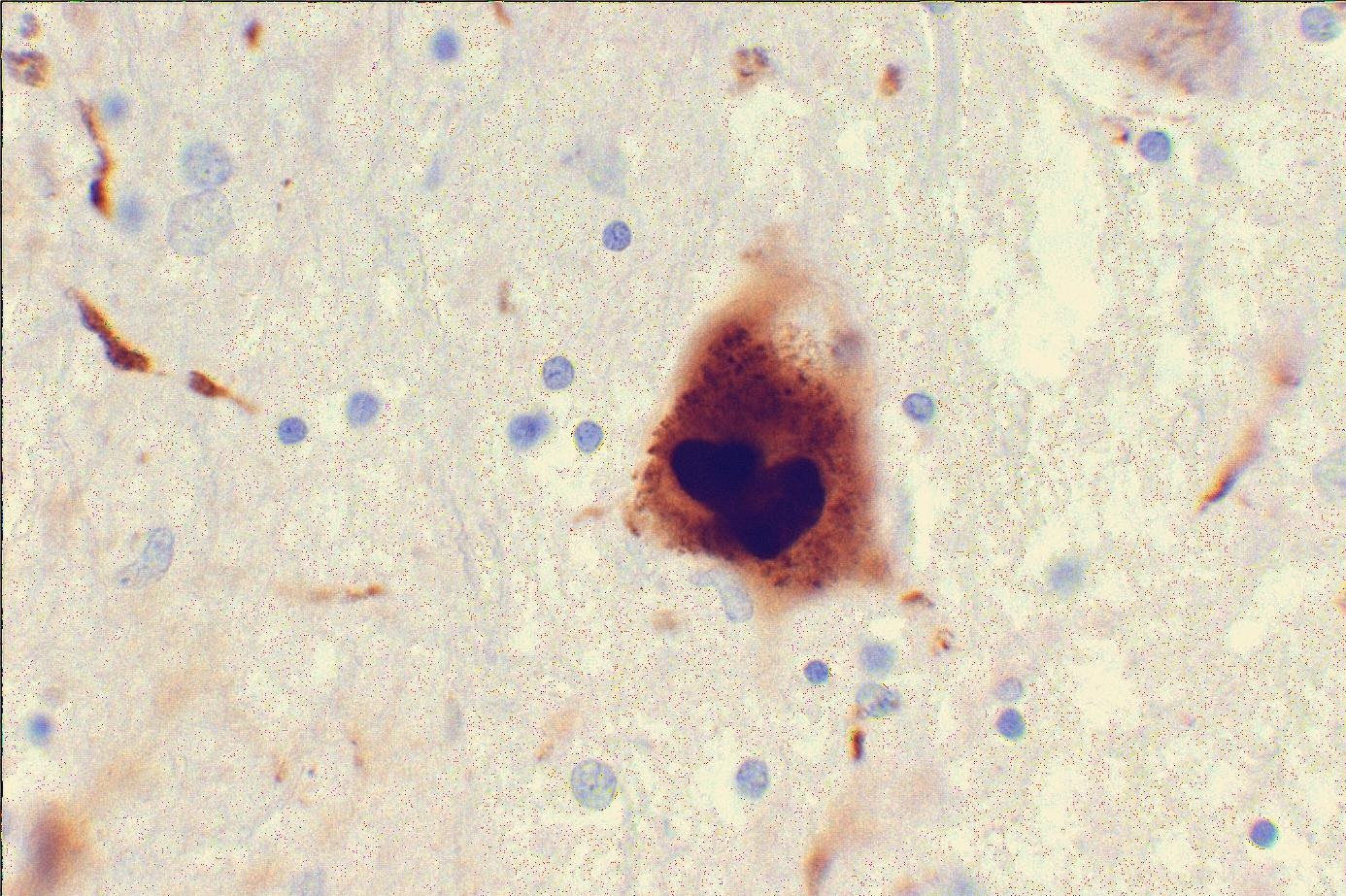
For the last year of her PhD, Anastasia has yet another project planned. Exposure of the ENS to bacterial curli proteins might induce the misfolding of alpha-synuclein, one of the protein aggregates that are associated with Parkinson's disease. These aggregates are then believed to spread to the brain much like prions. The project has just started and Anastasia hopes to get results before her PhD ends. "If we see alpha-synuclein aggregation after long term exposure to curli, along with immunometabolic changes in the ENS cells, that would be of great interest in our field. But I'm already satisfied with everything that I have done so far."
Working in both a pharmacology and a metabolomics group has taught her the best of both worlds, Anastasia says. "My cells are here in the pharmacology department but I move between the two labs and I've learned a lot from both."